They were admitted to hospitals with heart attacks, kidney failure, or due to psychiatric crises. They left with covid-19 if they did.
More than 10,000 patients were diagnosed with covid in hospitals in the United States last year, after being admitted for another cause, according to federal and state records analyzed exclusively for KHN.
But in fact, the number is an undercount, including most patients 65 and older, plus California and Florida patients of all ages.
However, among the possible scenarios that can go wrong in a hospital, it is a catastrophic figure: about 21% of patients who contracted covid in the hospital from April to September of last year died, data shows. In contrast, nearly 8% of other Medicare patients died in the hospital at that same time.
Steven Johnson, 66, was hoping to be released from an infection that made his hip raw at Blake Medical Center in Bradenton, Florida, last November. The retired pharmacist had survived colon cancer and was meticulous to avoid contracting COVID.
He couldn’t have known that, from April to September, 8% of that hospital’s Medicare covid patients were diagnosed with the virus after being admitted for another medical need.
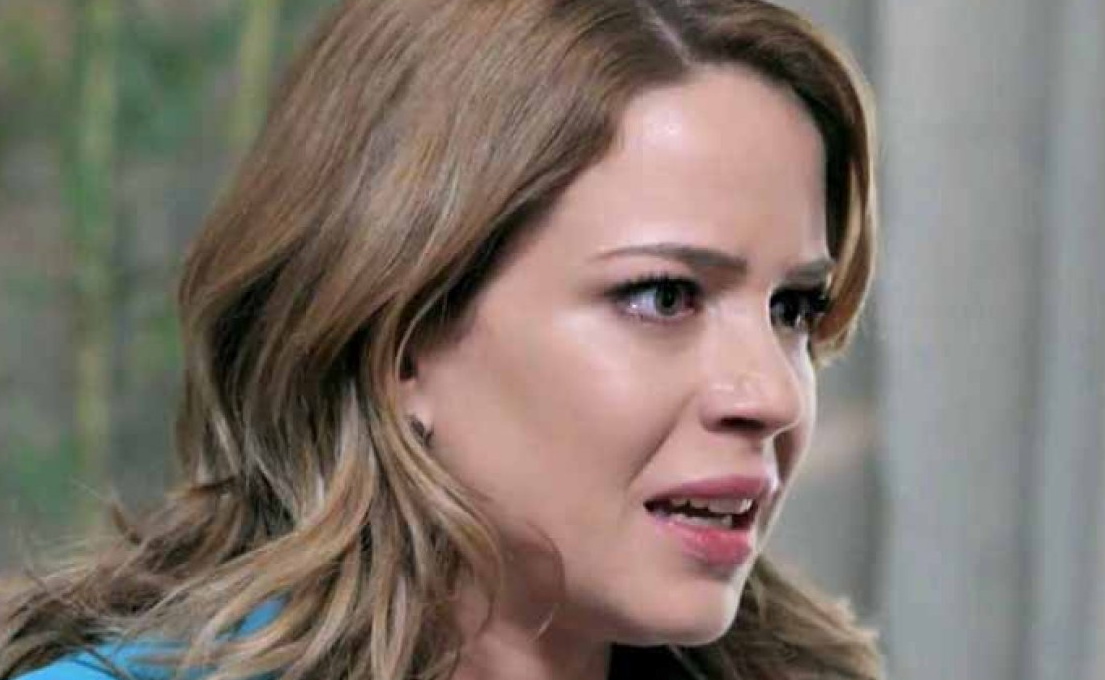
Johnson had tested negative for covid two days before being admitted. His wife, Cindy Johnson, also a retired pharmacist, said that after 13 days in the hospital, she tested positive.
Within hours, he was struggling to clear glue-like phlegm from his lungs. A medical team was barely able to control her pain. They asked Cindy to express her last wishes. She asked him: Honey, do you want to be intubated? He responded emphatically. He died three days later.
After her husband tested positive, Cindy Johnson, trained in contact tracing, quickly got tested for COVID. It tested negative.

But she kept thinking about a large number of hospital staff coming in and out of her husband’s room, often removing his mask, and she suspected that a staff member had infected him.
That the hospital, part of the HCA Healthcare chain, has not yet mandated vaccines is appalling, he said. I’m furious, she added.
How can you say on your website that ‘the security precautions we have put in place make our facilities among the safest possible places to receive medical care right now? he asked himself.
Lisa Kirkland, a spokeswoman for Blake Medical Center, said the hospital is strongly encouraging vaccination, noting that it follows federal guidelines from the Centers for Disease Control and Prevention (CDC) and state standards to protect patients.
President Joe Biden has called for all hospital employees to be vaccinated, but the requirement could face resistance in a dozen states, including Florida, that have banned vaccination mandates.
Overall, the in-hospital spread rate between Medicare and other patients was lower than in other countries, including the UK, which makes such data public and openly discusses it.
On average, about 1.7% of covid patients admitted to hospitals in the United States were diagnosed with the virus at these facilities, according to an analysis of Medicare records from April 1 to September 30, 2020, provided by Dr. James Kennedy, founder of CDIMD, a Nashville-based data analytics and consulting firm.

However, the infection rate was much higher at 38 hospitals where 5% or more of Medicare covid cases were documented as hospital-acquired.
The data comes from a challenging time period last year when protective equipment was in short supply, and testing was either poor or slow to produce results. Medicare data for the fourth quarter of 2020 and this year is not yet available, and the state data reflects from April 1 to December 31, 2020.
A KHN review of workplace safety records, medical literature, and interviews with high-spreading hospital staff indicates why the virus took hold: Hospital leaders were slow to admit it was airborne, making coughing patients dangerous to roommates and staff members, who often wore less protective surgical masks instead of N95.
Hospitals were unable to test all admitted patients, thanks to CDC guidance that left such testing to the facility’s discretion. Management often failed to inform workers when they had been exposed to covid and therefore was at risk of spreading it themselves.
The spread between patients and staff seemed to go hand in hand. At Beaumont Hospital, Taylor, Michigan, 139 covid infections were recorded in employees between April 6 and October 20 last year, a hospital inspection report shows. Nearly 7% of Medicare patients with covid tested positive after being admitted to that hospital for another cause, federal data shows.
A hospital spokesman said the tests were not available to evaluate all patients last year, resulting in some late diagnoses.
He said that now, all admitted patients are evaluated.
Tracking covid within healthcare facilities is not a new task for federal officials, who publicly report new cases each week in employees and residents in every nursing home across the country.
However, the Department of Health and Human Services reports data on the spread of covid in hospitals only at the state level, so patients do not know which facilities present cases.
KHN commissioned an analysis of hospital billing records, which are also used more widely to detect various hospital-acquired infections. For covid, the data has limitations. It can detect some community-acquired cases that were slow to appear, as it can take two to 14 days from exposure to the virus for symptoms to appear, with an average of four to five days.
The records do not take into account cases picked up in an emergency room or diagnosed after a patient is discharged from the hospital.
Linda Moore, 71, tested positive at least 15 days after a hospital stay for spinal surgery, according to her daughter Trisha Tavolazzi.

His mother was at Havasu Regional Medical Center in Lake Havasu City, Arizona, which did not have an above-average internal spread rate last summer.
The hospital implemented rigorous health and safety protocols to protect all of our patients during the pandemic, said Corey Santoriello, a spokesman for the hospital, who declined to comment on Moore’s case, citing privacy standards.
Moore was airlifted to another hospital, where her condition only worsened, her daughter said. After the fan was removed, she clung to life erratically for five and a half hours, while her daughter prayed that her mother would find her way to heaven.
“I asked his mom, his dad, and his family, and I prayed to God: Please come
show him the way,” Tavolazzi said. I relive that moment every day.
When Tavolazzi searched the hospital for answers about where his mother contracted the virus, he said he didn’t get any: No one called me back.
From two negative tests for covid to being the “zero patient”
When the second wave of covid subsided last September, doctors at the prestigious Brigham and Women’s Hospital published a reassuring study: with careful monitoring of the infection, only two of 697 covid patients acquired the virus at the Boston hospital. That’s about 0.3% of patients, about six times lower than the overall Medicare rate.
Brigham screened every patient he admitted, beating the CDC’s recommendations. He was transparent and open about security concerns.
But the study, published in the journal JAMA Network Open, sent the wrong message, according to Dr. Manoj Jain, an infectious disease physician and adjunct professor at Emory University’s Rollins School of Public Health. Covid was spreading in hospitals, he said, and the study buried the problem under the rug.
Shortly after publication, the virus began a stealth streak through the elite hospital. He came in with a patient who tested negative twice but turned out to be positive. She was patient zero in an outbreak that affected 38 employees and 14 patients, according to a study in the Annals of Internal Medicine originally published on Feb.9.
The authors of that study sequenced the genome of the virus to confirm which cases were related and exactly how it spread throughout the hospital.
As patients were moved from room to room in the early days of the outbreak, covid spread among roommates 8 out of 9 times, likely through aerosol transmission, according to the study.
A survey of staff members revealed that those who cared for coughing patients were more likely to get sick.
The virus also appeared to have bypassed CDC-supported protective equipment. Two staff members who had close contact with patients while wearing a surgical mask and face shield also became infected.
The findings suggested that the safer N95 respirators could help protect personnel.
Brigham and Women are now tested all patients upon admission, and again shortly thereafter. Nurses are encouraged to retest if they see a subtle sign of covid, said Dr. Erica Shenoy, associate chief of the Infection Control Unit at Massachusetts General Hospital, who helped develop the standards in Brigham.
Shenoy said that nurses and environmental service workers are sitting at the policy-making table: I personally make sure to say: Tell me what you are thinking, Shenoy said. There will be no consequences because we need to know.
The CDC guidelines, however, left a wide margin on protective gear and testing. To this day, Shenoy said, hospitals employ a wide range of policies.
The CDC said in a statement that its guidelines provide a comprehensive and layered approach to preventing the transmission of SARS-CoV-2 in healthcare settings and include testing patients who have even mild symptoms or recent exposure to someone with covid.
Infection control policies are rarely obvious to patients or visitors, beyond asking them to wear a mask. But reviews of public records and interviews with more than a dozen people show that in hospitals with high rates of spread of covid, staff members were often alarmed by the lack of safety practices.
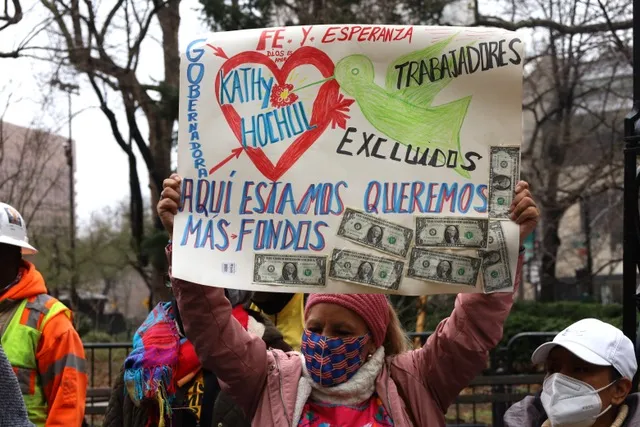
Nurses sound the alarm about the spread of covid. When covid arrived in Florida in the spring of 2020, nurse Victoria Holland confronted managers at the Blake Medical Center in Bradenton, where Steven Johnson died.
She said she was suspended early in the pandemic after participating in a protest and having a fit of anger when she was denied a new N95 respirator before a procedure that involved generating airborne particles.
The CDC warns that these procedures can spread the virus through the air.
Before the pandemic, nurses were trained to dispose of an N95 after each encounter with a patient.
When the suspension ended, Holland said, he felt insecure. “They didn’t tell us anything,” he said. “It was all a rumor among the doctors. If you had potential covid patients you would get a little surgical mask because [they didn’t] want to waste an N95 unless they knew the patient was positive. “
Holland said he resigned in mid-April. Her nursing colleagues filed a complaint with the Occupational Safety and Health Administration (OSHA) in late June alleging that staff “working around potential positive Covid-19 cases” had been denied PPE. Staff members protested in front of the hospital in July and filed another OSHA complaint that said the hospital was allowing covid-exposed employees to continue working.
Kirkland, Blake’s spokesman, said the hospital responded to OSHA and no deficiencies were identified.
Medicare’s analysis shows that 22 of 273 covid patients, or 8%, were diagnosed with the virus after being admitted to Blake. That is about five times higher than the national average.
Kirkland said there is no standard way to measure hospital-associated COVID-19 transmissions and that there is no evidence to suggest that the risk of transmission at Blake Medical Center is different than it would be found in other hospitals.
In Washington, DC, 34 Medicare patients with covid contracted the virus at MedStar Washington Hospital Center, or nearly 6% of their total, the analysis shows.
Dissatisfied with safety practices, which included gas sterilization and reuse of N95s, members of National Nurses United protested in the hospital garden in July 2020. At the protest, nurse Zoe Bendixen said a nurse had died because of the virus and 50 had become ill:
[Nurses] can become a source of disease transmission to other patients, coworkers, and family members.
Nurse Yuhana Gidey said she contracted covid after treating a patient who turned out to be infected. Another nurse, not the staff doing the contact tracing, told her she had been exposed, she said.
Nurse Kimberly Walsh said in an interview that in September 2020 there was an outbreak in a geriatric unit where she worked. He said management blamed the nurses for bringing the virus to the unit. But Walsh pointed to another problem: The hospital was not testing patients who came from nursing homes for covid, where the spread was rampant last year.
MedStar declined an interview request about its infection control practices and did not respond to specific questions.
While hospitals are required to track and publicly report rates of persistent infections such as C. diff, antibiotic-resistant staph, and surgical site infections, similar rates of hospital-acquired covid are not reported.
KHN examined a different source of data that Congress required hospitals to document about hospital-acquired conditions.
Data from Medicare, which indicates whether each covid case was present on admission or not, is available months after hospitalization in obscure files that require a data use agreement that is usually granted to researchers.
KHN counted cases, as federal officials do, in some cases where documentation is deemed insufficient to categorize a case.
For this data, considering a hospital-acquired COVID case falls to medical coders who review doctors’ notes and discharge summaries and ask doctors questions if the status is unclear, said Sue Bowman, senior director of coding and compliance policy of the American Health Information Management Association.
He said medical coders are aware that the data is used for hospital quality measures and would be careful to review contact tracing or other information in the medical record.
If a case was in the data that KHN used, that would mean it was acquired during the hospital stay, either from a healthcare worker or another patient or perhaps if a hospital allowed visits, from a visitor, Bowman said. That would be a fair interpretation of the data.
The high death rate for those diagnosed with covid during a hospital stay, around 21%, reflects the death rate of other Medicare covid patients last year when doctors had few proven methods to help patients.
It also highlights the danger posed by unvaccinated staff to patients, said Jain, the infectious disease physician. The American Hospital Association estimates that about 42% of the nation’s hospitals have required that all staff members be vaccinated.
We don’t need [unvaccinated staff] to be a threat to patients, Jain said. The [hospital] administration is too afraid to put pressure on the nursing staff, and the general public has no idea of the threat that an unvaccinated person poses to a vulnerable population.
Cindy Johnson said the hospital where she believes her husband contracted COVID faced minimal scrutiny in a state inspection, even after she herself reported that her husband had contracted COVID at the facility.
Johnson explored the possibility of suing but was told by an attorney that it would be nearly impossible to win such a case. A 2021 state law requires that proof of “at least gross negligence prevail in court.”
Johnson did ask a doctor who sees patients at the hospital: Please remove the big sign that says “OPEN AND SAFE.” In a matter of days, the poster disappeared.